By Heather Thompson
Undergraduate Student, University of Virginia
 George Washington’s financial papers detail a wide variety of medical transactions, many of which include very different substances or uses than would be familiar today. Navigating this may seem difficult to someone who has not studied colonial medicine. So, this page is intended to provide context and insight into these types of transactions.
George Washington’s financial papers detail a wide variety of medical transactions, many of which include very different substances or uses than would be familiar today. Navigating this may seem difficult to someone who has not studied colonial medicine. So, this page is intended to provide context and insight into these types of transactions.
Medicine prior to and during George Washington’s time was viewed differently than it is today. For example, there was a brief period in the 1770s when Virginia banned inoculation against smallpox.[i] For many of our Founding Fathers, illness and tragedy were an normal component of general life.[ii] Unfortunately, some of the medical solutions of the time did more harm than good.
NATURAL CURES
Many of the medicinal herbs and treatments casually mentioned in Washington’s financial records are not part of today’s modern medical dialogue. But that does not necessarily mean that these natural medicines are unsound or useless. In fact, modern aspirin derived from willow bark and penicillin from fungus.[iii] However, many of these remedies became problematic when used on patients.
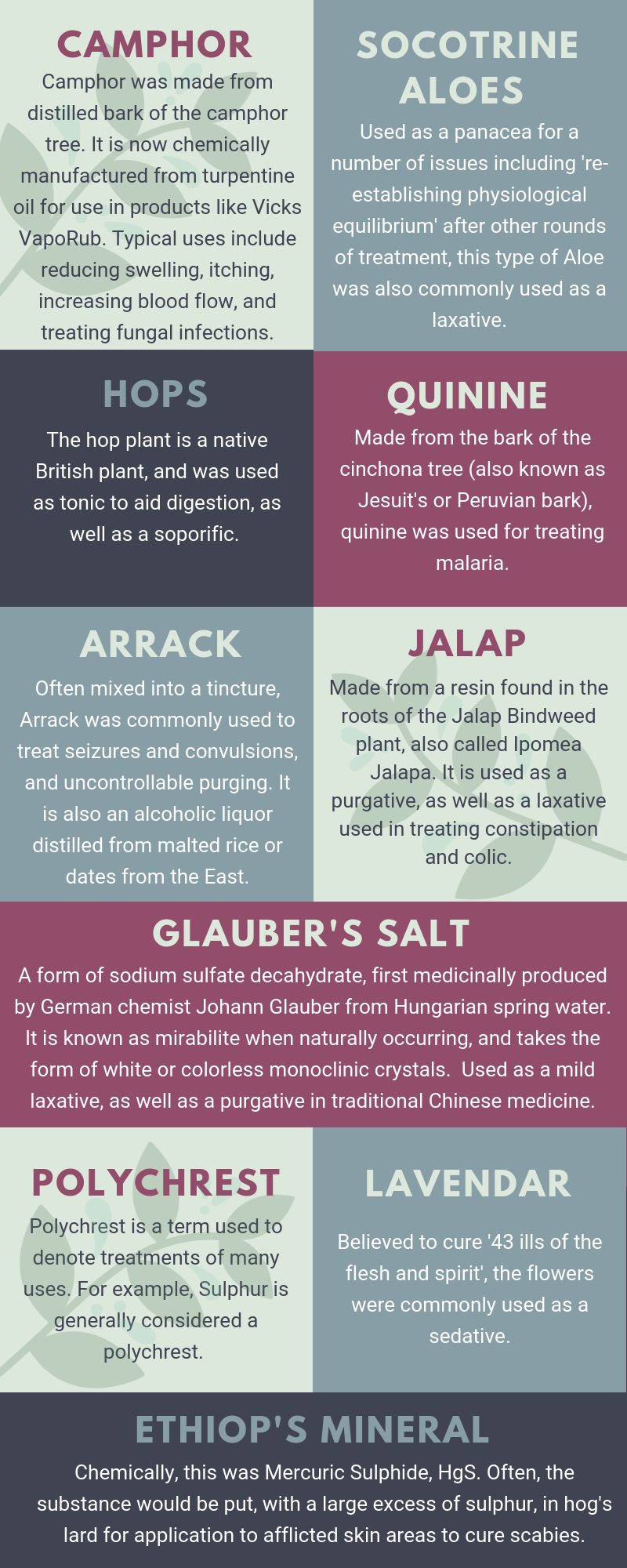
Washington’s financial papers mention a wide variety of various herbs and common tinctures. [iv] Such medications included opium, digitalis, foxglove, jalap, thyme, lavender, and calomel. The infographic here illustrates some of the most prominently used medicinal herbs from Washington’s time.
In addition to these medications were a number of archaic practices, which at times only expedited the death of a patient. For example, bloodletting was a common and widely accepted practice, but it was often detrimental to patients who were already ill. The death of George Washington himself was linked to infection and shock caused by excessive bloodletting.[v]
MEDICINE AND IDEAS FROM THE GLOBAL WEST
The medicines and treatments purchased by George Washington offer us a closer look at contemporary global engagement and trade patterns. Many of these cures originated in very different regions of the world.
For example, 'bark decoction,' which was often used to combat malaria, was ordered in two-pound quantities by Washington from England prior to the American Revolution.[vi] In 1759, Washington ordered drugs from London, including mercurous chloride, ipecac, lavender, and cinnamon water.[vii] Another concoction, Glauber’s salt, originated from a mid 17th-century German chemist who used Hungarian spring water.[viii] Camphor originated in Japan, opium in Turkey, and ipecacuanha in Brazil.[ix]
Not only were the medicines themselves exported, but the science of their uses was as well. The first medical school within the thirteen colonies was the University of Pennsylvania School of Medicine, which was founded in 1765. It offered "anatomical lectures" and courses on "the theory and practice of physik."[x] Many of the lecturers had studied at the University of Edinburgh before coming to the United States.
Despite these advancements and the global reach of knowledge, "the generality of people lay too much stress upon Medicine, and trust too little to their own endeavours. It is always in the power of the patient, or of those about him, to do as much towards his recovery as can be effected by the physician."[xi] In general, the early 18th-century colonists did not put much faith in their doctors either. Nevertheless, the contemporary medical approach was still leaps and bounds ahead of earlier theories.
 DEVELOPING THEORIES OF MEDICINE
DEVELOPING THEORIES OF MEDICINE
Ancient Greek philosophy laid the foundations of modern healthcare. The theory upon which colonial medicine was based goes as far back as Hippocrates in 460 B.C. He is widely recognized for his emphasis on ethical medicinal practices and strong scientific inquiry. [xii] Hippocrates made some groundbreaking advances within the field; for example, he characterized a number of mental illnesses with terms that we still use today. But some of his other ideas have proven to incorrect, such as the concept that intelligence and sensitivity reach the brain through the mouth via breathing.[xiii]
From there, a number of theorists contributed to the changing (and largely inaccurate) cannon of medical knowledge leading up to the 18th century. Galen, a Greek physician born in 120 A.D., was one of the next influential individuals. Galen developed the four "humors," based on Aristotle’s writings in 350 B.C. Aristotle believed that the four elements made up everything on Earth and that the goal of the practitioner was to restore a harmonious equilibrium between the relevant elements.[xiv] Until the Renaissance, the Western world lacked a focus on medical innovation and effective treatment solutions. Paracelsus was a 16th-century Swiss physician who made significant contributions with his theories of mineral cures based largely in astrology; his theories involved shifting "astral forces" in order to cure individuals.[xv] The Age of Enlightenment during the 18th century finally brought with it the advent of what we might consider modern medicine. Eventually, Leyden, Paris, Montpellier, Cambridge, and Oxford became known as the best places in Europe to learn medicine.[xvi]
However, even by the 18th century, “advanced medical ideas often stemmed from educated laymen like Jefferson and the other American founders… rather than physicians, who often had little to offer seriously ill patients.”[xvii]
SLAVE MEDICINE
The role of enslaved Africans in colonial medicine is often neglected in discussions of colonial medicine but is just as important. For the most part, the colonial laws that applied to slaves similarly affected the rest of the population. However, one notable exception was "the administration of poisonous medicines," which had special provisions dealing with slaves.[xviii] This latter restriction arose due to the belief that many slaves practiced witchcraft and tribal medicine brought from Africa. A section of 1748 code even allowed capital punishment for a “Negro” who "prepared and administered medicine of any sort unless their owner had consented".[xix] Between 1780 and 1864, fifty-eight slaves in Virginia were convicted of poisoning or attempted poisoning.[xx] Traditional Western medical strategies included a large degree of cutting, bleeding, and amputating in order to heal the afflicted. These cures were foreign to many Western African healing traditions and often regarded as dangerous by slave populations.[xxi] Thus, despite such harsh penalties, slaves continued to practice traditional West African medicine.
In fact, “Negro medicine,” as it was commonly referred to, epitomized the increasingly globalized nature of healthcare. Given the ineffectiveness of some traditional European cures, many slave owners allowed slave "healers" to conduct their own medicine on slaves, and at times even on owners and their families.[xxii] The health of slaves was critical to the economic success of plantation owners. So, if it was found that treatments developed from West African traditions were effective, there was a clear incentive for the owners to allow such practices.[xxiii] A "negro doctor" thus referred to a slave who administered medicine to other slaves, and occasionally to whites as well. "Negro doctoresses" were usually women who acted as midwives and administered medicinal herbs.[xxiv]
Slaves brought West African healing traditions across the Atlantic in more ways than one. In addition to the travel of the practice, the plants themselves were (both intentionally and unintentionally) transferred to the New World. Some plants, such as liquorice seeds, were transported via necklaces intended to serve as protective amulets. Others came within the straw that commonly lined ships' holds as they transported slaves to the colonies.[xxv]
Plants were also often combined with religious rituals and prayer as a necessary component of the healing process within slave medicine. This was often at odds with Christian colonists, who viewed these "witch doctors" and "conjurers" as casting dangerous spells. However, on occasion, white doctors who saw the medicinal practices of enslaved individuals working effectively would adopt the same strategies. In the late 18th-century, Dr. Richard S. Cauthorn announced in the Monthly Stethoscope that an old folk remedy historically used by blacks in the counties north of Richmond worked to treat fever almost as well as quinine.[xxvi]
WASHINGTON’S DOCTORS
George Washington received care from a number of doctors throughout his life, nine of which are mentioned at some point within his financial papers that are transcribed so far.
One of Washington’s chief physicians was Dr. James Craik. Hailing from Scotland, Craik studied medicine at the University of Edinburgh before coming to the United States. The two men became close friends after Craik was appointed surgeon of Washington's Virginia Regiment in 1754. Later, Craik became deputy director general of the hospitals in the middle department in May 1777 at Washington's recommendation. Craik worked as Washington's medical officer during the French and Indian War, and as chief physician of the army from 1781 to 1784.[xxvii] From 1797 to 1799, Craik served as primary doctor to Washington as well as to his household and various connections, which amounted to more than 300 people.[xxviii]
According to Washington’s financial records, Craik attended to the needs of the Washington family and laborers across all five farms (Mansion House, River, Union, Dogue Run, and Muddy Hole), charging one pound (roughly three dollars) per visit.[xxix] It is also surmised that Craik waived a number of bills towards the end of Washington's life due to his inability to pay, and because Washington funded the education of Craik's son in 1788.[xxx] Craik generally charged three shillings for bleeding, which he (along with many doctors of the time) seems to have viewed as a universal panacea for any illness.[xxxi]
 COLONIAL GENDER ROLES AND MIDWIVERY
COLONIAL GENDER ROLES AND MIDWIVERY
Of forty-two financial entries that record the services performed by Craik, there was only one reference to obstetrics. Typically, obstetrical procedures were left to women, specifically midwives. Despite women's active roles in medical treatment, medicinal practice can at the same time demonstrate the semi-adaptive dichotomy of colonial gender roles.
While women were less engaged in the "theory of medicine" and its development, most women practiced medicine in some form.[xxxii] Women primarily served as midwives and obstetricians in the field referred to as "domestic medicine." Domestic medicine encompassed practices, such as childbirth, which frequently occurred in the home rather than a hospital or clinic.[xxxiii] Elite women were often able to care for the indigent within their localities and also use their medical knowledge in order to make influential connections with powerful men. [xxxiv]
The beginning of the Revolutionary War marked a definite change in the scope of a women’s role both within the family and within the community. However, a job as a Revolutionary War nurse brought many hazards, including relegation to the dirtiest jobs, exposure to various deadly diseases in unsanitary conditions, and threats of ration reduction if the nurse requested to switch jobs.[xxxv]
A POSITIVE FINAL NOTE
Much of this article paints a relatively gloomy picture of the rudimentary nature of colonial medicine. However, it should be noted that while by modern standards, there was much to be desired, this was still an era of great improvement. Historian Peter Gay notes,“The most tangible cause for confidence lay in medicine … Medicine was the most highly visible and the most heartening index of general improvement.”[xxxvi]
[i] Wall, Charles C. "”Dr. His Excly Geo. Washington to James Craik": Notes on a Medical Bill." The Virginia Magazine of History and Biography 55, no. 4 (1947): 324, http://www.jstor.org/stable/4245506
[ii] Abrams, Revolutionary Medicine, 4.
[iii] ibid, 17.
[iv] The Edinburgh Medical and Surgical Journal, Volume 16, Publ. Arch. Constable & Comp., 1820.
[v] Abrams, “Revolutionary Medicine”, 8
[vi] Wall, “Dr. His Excly”, 328
[vii] Abrams, “Revolutionary Medicine”, 18
[viii] Ibid, 17
[ix] “"Colonial Medicine", Jamestown-Yorktown Foundation, Williamsburg, Virginia, www.historyisfun.org/pdfbooks/colonial_medicine.pdf, page18
[x] McConaghy, Mary D. "School of Medicine: Historical Development, 1765-1800." University of Pennsylvania University Archives and Records Center. http://www.archives.upenn.edu/histy/features/1700s/medsch.html2017).
[xi] Buchan, William. Domestic Medicine; Or. Philadelphia: Printed for Joseph Crukshank, Robert Bell, and James Muir, 1784.
[xii] Hughes, Thomas P. "Medicine in Virginia 1607-1699." 21 (1957).
[xiii] Kleisiaris CF, Sfakianakis C, Papathanasiou IV. "Health care practices in ancient Greece: The Hippocratic ideal." Journal of Medical Ethics and History of Medicine. 2014;7:6.
[xiv] Ibid, 22.
[xv] “Colonial Medicine”, 19
[xvi] Hughes, Thomas P. "Medicine in Virginia 1607-1699." 21 (1957).
[xvii] Abrams, “Revolutionary Medicine”, pg. 17
[xviii] Tate Jr., Thad W. April, 1957. The negro in eighteenth-century williamsburg. Williamsburg: Colonial Williamsburg Foundation Library, Colonial Williamsburg Foundation Library Research Report Series – 0121, page 127.
[xix] Mays, David J., Edmund Pendleton, 1721-1803; A Biography (Cambridge, Mass., 1952), I, 42-44
[xx] Andrae, Christine “Slave medicine”, 2009, Monticello: Robert H. Smith International Center for Jefferson Studies, pg. 1.
[xxi] Ibid,, pg. 1.
[xxii] Ibid, pg. 4.
[xxiii] Fillmore, Randolph, "The Evolution of the U.S. Healthcare System", Science Scribe, 336-338, www.sciencescribe.net/articles/The_Evolution_of_the_U.S._Healthcare_Syst...
[xxiv] Andrae, Christine, “Slave medicine”, pg. 2.
[xxv] Ibid, pg. 3.
[xxvi] "Colonial Medicine", page 20
[xxvii] Wall, “Dr. His Excly,” 318
[xxviii] Ibid, 319
[xxix] Ibid, 319
[xxx] Ibid, 320
[xxxi] Ibid,, 323
[xxxii] Abrams, “Revolutionary Medicine”, 18
[xxxiii] Fillmore, Randolph, "The Evolution of the U.S. Healthcare System", page 337.
[xxxiv] Tannenbaum, Rebecca J., "The Healer's Calling - Women and Medicine in Early New England", Cornell University Press, Feb. 11, 2009, 162.
[xxxv] "Women's Service with the Revolutionary Army", Colonial Williamsburg, 2017, www.history.org/history/teaching/enewsletter/volume7/nov08/women_revarmy...
[xxxvi] Abrams, “Revolutionary Medicine”, 2